An ounce of prevention is worth a pound of appeal
Comprehensive clinical denials management is a game of both offense and defense. On offense, the healthcare provider strives to code, bill and submit clean claims that receive prompt payment. Providers win by preventing denials and downgrades. On defense, the provider protects revenue by appealing denied claims and reinforcing appeals with evidence refuting the denial. Although it requires both a strong offense and defense to manage denials effectively, prevention is generally the first step forward.
Identify denial risks to strategically deploy resources
With revenue at risk in multiple areas of reimbursement, denial prevention requires a holistic view of hospital operations, both clinical and administrative. Healthcare providers face a serious financial threat from the rise of targeted denials, so every revenue-generating department and service must receive attention.
Keep up to date with coding rules and regulations
With the increasing ownership of physician practices by health systems, the risk to coding and billing evaluation and management services is increasing. New rules for hospital-based physician coding of their visits that go into effect January 1, 2023, may remedy this somewhat. Teaching physicians the new coding rules is important because it can not only reduce revenue risk but also improve the overall quality of clinical documentation.
Focus on high cost and utilization targets
Always consider the care setting for a treatment or procedure as payers tend to favor ambulatory surgery centers for their lower cost and use that as a basis for denials if the same care is delivered in a hospital setting. Because of the very high cost of many oncology drugs, infusions are receiving more scrutiny from payers to ensure medical necessity, indication for the disease, and even proper dosage. All infusion clinics should have oversight to ensure those things are reviewed for absolute accuracy. Imaging is another high denials risk area and as for labs, the areas where there can be denials because of questioned medical necessity are too numerous to count.
Monitor reimbursement to find revenue leaks
On the hospital side, we see the emergency department being targeted for denials with payers using automated facility fee downgrade algorithms. These don´t appear as denials but as payment reductions, making them difficult to detect and correct if providers aren´t monitoring for them. Keep an eye on evaluation and management services like observation. Medicare has one set of rules for observation, while private payers use their own rules, so knowing which rule set applies really matters for revenue integrity.
Watch for strategic DRG downgrade targets
Looking at inpatient revenue risk, DRG downgrades are becoming more prevalent as a payer strategy. Successfully downgrading a DRG benefits payers by lowering the cost of other services tied to the lower weighted DRG. Long term acute care hospital (LTACH) transfers and acute rehab denials are also becoming more common. Especially with Medicare Advantage plans, there is pressure to not approve transfers to LTACH and acute rehab. Perhaps as fallout from COVID-19 when psychiatric care was in high demand, those services are also being closely scrutinized and should be monitored for denials trends and reasons.
The three faces of medical necessity
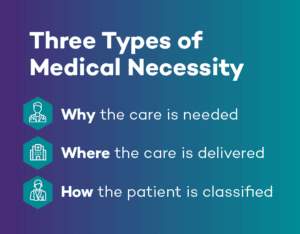
With so many denials now based on questioning the broad term medical necessity, it’s important to know there are three types of necessity at play. First, can the physician prove that care was required and appropriate? This is where proper clinical documentation of diagnosis tied to recommended treatment pays dividends for preventing denials. Second is necessity of setting – can the service be performed with the same clinical outcome at a lower cost in a different setting like an ASC? If so, it should be. Finally, payers will look at necessity of status. If a patient can receive care as an outpatient rather than inpatient at a lower cost, that becomes the preferred option.
Build a team and give them the right tools
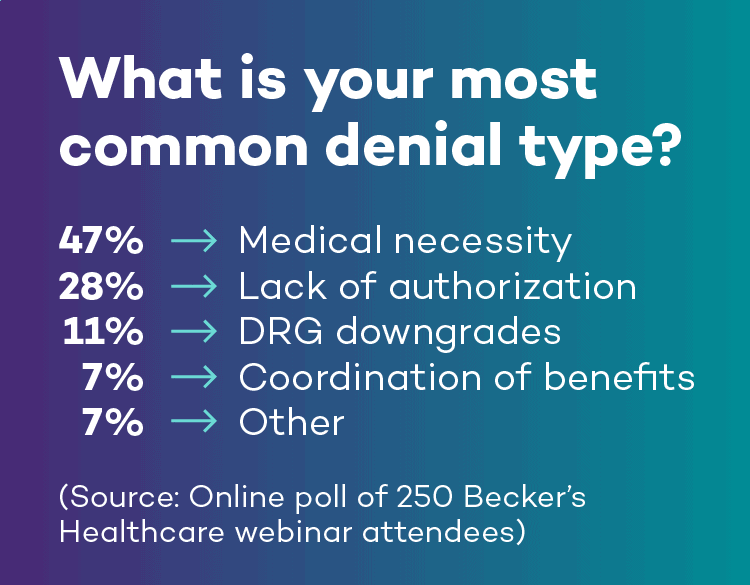
Knowledge is power, and the more you know about what’s causing denials the better you can respond and defend your billed charges as medically necessary, clinically appropriate, and correctly coded. This should start by doing a thorough root cause analysis of denials. Payers will deny claims for a wide variety of clinical reasons like medical necessity as well as administrative reasons like lack of prior authorization. But our data shows they tend to target certain diagnostic codes based on their own data analysis.
Because the causes of denials are so far ranging, the most important management best practice is to assemble a cross-disciplinary team of stakeholders to manage the process. The team should meet regularly to talk about denials trends, causes, and prevention measures and ensure denials are being addressed in the most effective way.
Negotiate payer contract language to protect revenue
On the subject of managed care contracts, providers should ensure to negotiate as much favorable language as possible and never make any reimbursement requirement more rigorous or stringent than the prevailing regulatory guidance. Not every service is covered by every payer or plan, despite it being reimbursed by Medicare and Medicaid or approved by the FDA – ultimately reimbursement all comes down to the terms defined in each payer contract.
Creating a payer matrix is another best practice that can make appeals much more efficient. The payer matrix has rows for each payer and plan, and columns for essential information like filing timeframe, mailing address or portal location, and first and second appeal steps. Having all of those things in one place makes it much easier to follow process and file those appeals in a timely manner.
Appeal like an attorney for best results
While there’s no one right way to craft an appeal, following a formula that’s taught in law schools can provide a framework that presents your case in a highly effective way. The formula, P.L.E.A., encompasses the principles for effective appeals – persistence, logic, exculpation, and advocacy.
When it comes time to actually write the appeal, another formula, I.R.A.C., can be very helpful. This formula first examines the issue driving the denial, applies the rules governing the claim, analyzes the claim and denial, and offers a conclusion on why the appeal should be upheld.
More information about using the P.L.E.A. and I.R.A.C. formulas is available for download.
Drive quality improvement with analysis and education
Perhaps the most important point to remember about managing denials is to always close the process loop with analysis and education. Root cause reporting gives the interdisciplinary team the information it needs to educate staff on processes and workflows needing improvements. Denials prevention and management really go hand in hand. Denials is an evergreen pain point for providers, so be sure that denials prevention starts at the beginning with front-end registration, proceeds through quality clinical documentation, and always leverages a deep understanding of payers’ requirements to get services approved and delivered.
This post summarizes material from a Becker’s Healthcare webinar, Take Control of Clinical Denials, presented by Ronald Hirsch, MD, FACP, CHCQM, CHRI, Vice President of Regulations and Education at R1 RCM, and Sarah Mendiola, Esq., LPN, CPC, CPCO, Senior Vice President of Denials Management at R1, a R1 company.
To learn more about taking control of denials, visit https://www.r1rcm.com/what-we-do/revenue-recovery/denials-recovery/.